Healthcare Payers
Secure, compliant cloud solutions that streamline operations and empower better decision-making.

 Smarter processes,
Smarter processes,
fully secured data.
Processing claims, managing data, and staying ahead of compliance changes is no small feat.
Our secure, compliant cloud solutions, including our healthcare-specific CSPM platform and cloud operations, streamline operations, protect sensitive data, and reduce inefficiencies so you can focus on delivering value to your members.
From automating claims workflows to preventing fraud and ensuring data accuracy, we bring healthcare-specific expertise to simplify your day-to-day.
Trust ClearDATA to streamline
workflows and ensure data accuracy.With ClearDATA managing your cloud operations, you gain a trusted partner committed to your success and security.
Enter our
breach-free zone.

PHI records breached over 14 years in business under ClearDATA management, so you stay confident we’ll keep your member data secure in the cloud.
Recover at
lightning speed.

Faster Mean Time to Resolve (MTTR) by our team compared to doing it on your own, ensuring you protect claims processing and member services.
Stay effortlessly
compliant.

Average continuous compliance score of our customers, helping you adhere to HIPAA, HITRUST, and state regulations with automated security controls.
Slash costs,
streamline workflows.

Potential savings in cloud operations costs by working with ClearDATA, so you reduce risk and reinvest savings into better member experiences.
Here’s how ClearDATA works for you:
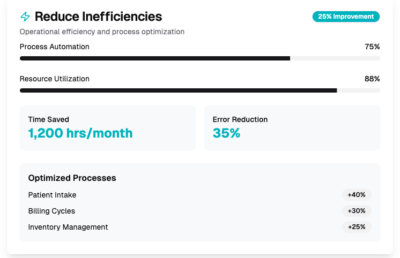
Reduce Inefficiencies
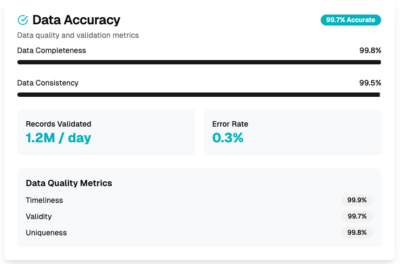
Data Accuracy
Fraud Detection
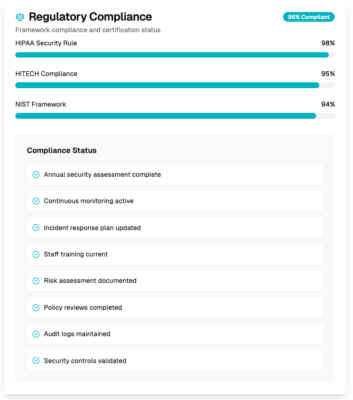
Regulatory Compliance
Claims processing and administrative inefficiencies:
Use our managed services to help you streamline claims processing and reduce administrative inefficiencies. We provide you the automation tools, workflow optimization, and data analytics capabilities to improve your claims management processes.
Credentialed. Celebrated. Certified.